About Us
Learn about the vision and purpose of the Robotics, Telesurgery and Surgical AI Initiative Collaborative Community.
Vision
The evolution of surgery has undergone remarkable transformations over the centuries, progressing from rudimentary procedures to highly advanced techniques. The history of surgery can be traced back to ancient civilizations, where simple surgical interventions were performed with primitive tools and limited knowledge. The Renaissance marked a significant shift with the emergence of anatomical studies, leading to improved understanding of the human body and more precise surgical procedures.
The 19th and early 20th centuries witnessed the advent of aseptic techniques and anesthesia, revolutionizing the safety and efficacy of surgeries. The mid-20th century saw the rise of open surgery, where large incisions were made to directly access and manipulate internal organs. While open surgery became the standard for decades, it was not without its drawbacks, including prolonged recovery times, increased risk of infection, and considerable patient discomfort.
The late 20th century witnessed a paradigm shift with the introduction of minimally invasive surgery (MIS), characterized by smaller incisions and the use of endoscopes and specialized instruments. This approach significantly reduced patient trauma, minimized scarring, and hastened recovery times. Laparoscopy became a common technique for various procedures, ranging from appendectomies to gallbladder removal.
In recent years, improving the precision of computer technology with the dexterity of a surgeon became a reality. Robotic surgery emerged as one such transformative concept when it was pitched to The Defense Advanced Research Projects Agency (DARPA) in the late 20th century. The idea was to leverage robotics to enhance surgical precision and minimize human error, particularly in high-stakes situations such as battlefield surgeries. Drawing inspiration from industrial robotics and remote-controlled devices, researchers proposed the development of minimally invasive surgical systems controlled by surgeons from a distance. This concept aligned with DARPA’s mission to push the boundaries of technology for strategic advantage. The initial investment and research in robotic surgery paved the way for the beginning of this revolutionary medical practice, which has since evolved into a cornerstone of modern surgical procedures, offering enhanced precision, shorter recovery times, and improved patient outcomes. Robotic surgical systems, such as the da Vinci Surgical System, enable surgeons to perform complex procedures with enhanced precision through small incisions.
The next frontier in surgical evolution is telesurgery, a revolutionary concept that leverages advanced telecommunication technologies. Telesurgery enables surgeons to perform procedures remotely, with the assistance of robotic systems and real-time communication. 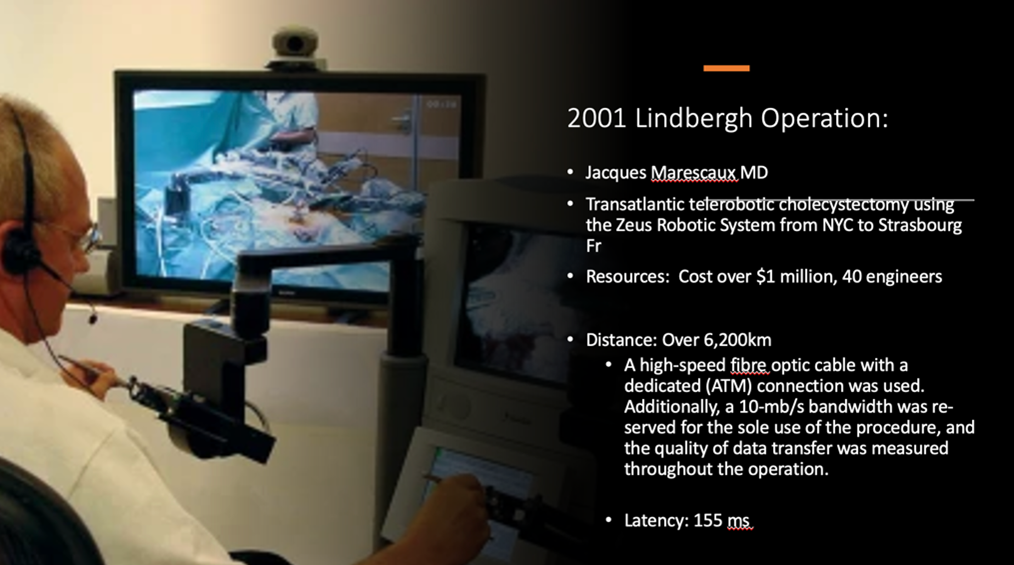 The first successful telesurgery, ‘Operation Lindbergh’, was performed by Jacques Marescaux and his team transatlantically, but costs to implement and maintain the practice, as well as increased technical challenges, were prohibitive and telesurgery delivery was paused. Today, with 5G networks and the state of global connectivity, telesurgery has become technically feasible. Many global robotic platform companies have been investing in making their devices telesurgery capable due to their aligned vision that it is the natural evolution of surgical practice. This could bridge geographical gaps, allowing expert surgeons to operate on patients located in remote or underserved areas, as well as respond swiftly to emergencies or time-sensitive procedures.
The first successful telesurgery, ‘Operation Lindbergh’, was performed by Jacques Marescaux and his team transatlantically, but costs to implement and maintain the practice, as well as increased technical challenges, were prohibitive and telesurgery delivery was paused. Today, with 5G networks and the state of global connectivity, telesurgery has become technically feasible. Many global robotic platform companies have been investing in making their devices telesurgery capable due to their aligned vision that it is the natural evolution of surgical practice. This could bridge geographical gaps, allowing expert surgeons to operate on patients located in remote or underserved areas, as well as respond swiftly to emergencies or time-sensitive procedures.
The deficit in skilled surgeons in many rural or impoverished areas of the world is significant with many highly populated areas lacking the expertise for critical procedures. Also, the health disparity in the world is vast, with drastic differences in the financial infrastructure 
 between different parts of the world. The lower-income countries have the least access to proficient medical and surgical care. It is estimated that more than 15 million additional healthcare professionals are required to achieve universal healthcare by 2030, whom should also be distributed evenly around the world. This would require an enormous investment in medical and surgical education globally. Telesurgery has the potential to improve surgical education by providing tele-mentoring to more surgeons globally. This has significant potential to improve surgical quality and reduce complications giving enormous humanitarian benefits. The network advancements However, despite significant improvement in technology, telesurgery also presents challenges related to latency, as well as ethical, financial, regulatory, legal and cultural implications.
between different parts of the world. The lower-income countries have the least access to proficient medical and surgical care. It is estimated that more than 15 million additional healthcare professionals are required to achieve universal healthcare by 2030, whom should also be distributed evenly around the world. This would require an enormous investment in medical and surgical education globally. Telesurgery has the potential to improve surgical education by providing tele-mentoring to more surgeons globally. This has significant potential to improve surgical quality and reduce complications giving enormous humanitarian benefits. The network advancements However, despite significant improvement in technology, telesurgery also presents challenges related to latency, as well as ethical, financial, regulatory, legal and cultural implications.
However with this great innovation also comes great responsibility. Our Executive Community issued a set of recommendations for the safe and responsible administration and practice of Telesurgery;
Prioritize Patient Safety and Efficacy
Maintain Transparency, Honesty & Consent
Foster Human Interaction and Empathy
Adhere to Ethical Medical Practices
Establish Clear Accountability and Liability
Uphold Data Privacy and Security
Promote Accessibility and Equity
Encourage International Collaboration and Standardization
Promote Continuous Education and Training
Promote Innovation of Safe & Trusted Telesurgery Technologies
As technology continues to advance, the integration of artificial intelligence (AI) into telesurgery may further enhance surgical capabilities. AI telecommunication optimization for example, can predict the gaps in the 5G networks, reroute and work around the the congestion. By learning from thousands of expert cases, AI can become an effective guide to younger surgeons when performing complex surgical cases in areas that lack experienced surgeons. The combination of robotic assistance, telecommunication, and intelligent automation holds the potential to redefine the landscape of surgery, making it more accessible, efficient, and precise on a global scale. Telesurgery represents a promising frontier that could revolutionize healthcare delivery and bring expert surgical care to patients in distant corners of the world.
Purpose
The Robotics, Telesurgery and Surgical AI Initiative Collaborative Community aims to recommend, best practices and robust strategies for addressing challenges in establishing remote surgery programs for equitable access to healthcare. One of the core foundations is generating and evaluating evidence that supports innovative approaches to remote surgical solutions while advocating patient rights and navigating the ethical, legal and regulatory conundrums that could arise. The community may also work to clarify ill-defined challenges or generate consensus on the definitions and scope of the obstacles that could be faced during launching and maintaining a functional robotic or remote surgery program. Another focus of the group would be validating and providing recommendations on various emerging robotic platforms entering the market, making sure they adhere to the standards required for safe and efficient surgery. By leveraging the wide variety of resources, power and expertise of the community members, the Robotics, Telesurgery and Surgical AI Initiative Collaborative Community can help address challenges and opportunities related to performing remote surgery on a national as well as an international scale.
Working Framework
Identifies Challenges and Opportunities
within the telesurgery and robotic realm, identifies key issues that need to be addressed in order to implement the program
Contacts Stakeholders
and builds evidence based and practical solutions, as well as outlines strategy and protocols for effective practice
Engages the Ecosystem
to act upon recommendations, standards, implementation guidelines
Observes the Impact
and learns from experience to build on
